Table of contents
- Main findings
- Summary
- Users and policy context
- Overview
- Data sources and linkage
- Gestational age
- Ethnicity
- Birthweight
- Age of mother at birth of baby
- Multiplicity
- Marital status and type of registration
- National Statistics socio-economic classification
- Cause of death groups: by gestational age and combined ethinc group
- Small for gestational age
- Downloadable tables
- References
- Background notes
1. Main findings
Babies born in 2013 had an infant mortality rate of 3.8 deaths per 1,000 live births, compared to 3.9 deaths per 1,000 live births for babies born in 2012.
Term babies had a significantly lower infant mortality rate (1.4 deaths per 1,000 live births) and pre-term babies had a significantly higher rate (21.1 deaths per 1,000 live births) compared to the overall rate.
Pakistani, Black Caribbean and Black African babies (6.7, 6.6 and 6.3 deaths per 1,000 live births respectively) had the highest infant mortality rates. This may be explained as these ethnicities are more likely to live in a deprived area and more likely to have parents in a less advantaged socio-economic position.
2. Summary
This bulletin presents figures on all births and infant deaths in England and Wales in 2013. The figures are based on birth registration information for babies born in England and Wales in 2013, linked to birth notifications data (using the NHS Numbers for Babies (NN4B)), and death registrations for babies who died before their first birthday and whose death were registered with us by the 20 July 2015. This birth cohort allows births and infant deaths to be reported by gestational age and ethnicity.
The infant deaths rates in this bulletin may differ slightly from those published in Deaths Registered in England and Wales, 2013 (DR) and Childhood, Infant and Perinatal Mortality in England and Wales, 2013 (CIPM). The infant mortality rate presented in DR, 2013 (4.4 deaths per 1,000 live births) was based on deaths that were registered in 2013. The rate in CIPM, 2013 (3.8 deaths per 1,000 live births) was based on deaths occurring in 2013 that have been linked to their birth registration details. These 2 rates were based on death cohorts.
Within this bulletin, a difference which is described as “significant” is statistically significant and has been assessed using 95% confidence intervals.
Back to table of contents3. Users and policy context
There is interest in infant deaths statistics from policymakers, those responsible for managing services for mothers and babies, charities and academics interested in research into causes of infant death.
Gestational age and ethnicity are not always collected at birth registration and we have only routinely reported them since 2006. The findings reported in this bulletin can help in understanding how these important factors relate to births and infant deaths.
We are the only source of National Statistics on gestation-specific infant mortality with ethnicity in England and Wales.
The Department of Health’s publication Healthy lives, healthy people: Improving outcomes and supporting transparency (DH, 2012) sets out a public health outcomes framework for England for 2013 to 2016. The domain “health improvement” includes the high level indicator “low birthweight of term babies” (indicator 2.1), which is defined as the percentage of all live births at term (37 weeks and over) with low birthweight (under 2,500 grams).
Infant mortality statistics for Scotland and Northern Ireland are the responsibility of National Records of Scotland and the Northern Ireland Statistics Research Agency respectively.
Please refer to background note 1 for definitions of terms used in this release.
Back to table of contents4. Overview
Substantial inequalities in infant mortality rates are known to exist between white and ethnic minority groups in England and Wales (Gray et al., 2009), and low gestational age is strongly linked to poor health (or mortality outcomes) (Kurinczuk et al., 2009). However, information about ethnicity and gestational age is not always collected at birth registration.
Since 2005 we have linked birth registration records with NHS birth notification records. These data are then further linked to death registration records for babies who died before their first birthday. By linking the 3 data sources, figures can be reported for infant mortality by gestational age and ethnicity, as well as other risk factors including: birthweight, mother’s age at birth of child, marital status and socio-economic status (based on the most advantaged parent’s occupation).
The NHS birth notifications system collects information about ethnicity to help organisations monitor their service delivery. Ethnicity is usually self-defined, for birth notifications the baby’s ethnic group is defined by the mother.
Individuals may choose not to state their baby’s ethnicity. In some areas with a very high proportion of “Not Stated” records opting-out may not be the sole reason for incomplete data, as the “Not Stated” response category also includes “not known”, “missing” and “not asked”. For babies born in 2013, 3.4% of live births had ethnicity recorded as “Not Stated”.
Low gestational age is a main risk factor associated with mortality in the perinatal period. Linking birth notifications data to information collected at registration allows gestational age to be analysed with other information routinely collected at birth registration.
For the purposes of this bulletin, if gestational age was below 22 weeks and birthweight was recorded as 1,000 grams or more, the data were considered invalid and were excluded from the analysis. For babies born in 2013, 0.3% of live births had no gestational age stated. Previously these “gestational age not stated” cases did not show any strong relationship with any other factor at a national level.
Back to table of contents5. Data sources and linkage
The Regional Director of Public Health must be notified of a birth within 36 hours by a doctor or midwife. At this point, the NHS Numbers for Babies (NN4B) system for recording birth notifications allocates an NHS number, and the doctor or midwife records the birth details that are not collected at birth registration.
All births in England and Wales must be registered within 42 days of occurrence. As well as details of the birth (date, sex, single or multiple birth), information is also collected about the parents for the public register and for statistical purposes, for example, mother’s usual residence and her age at the time of the birth. Information is collected about the second parent if the parents are married or in a civil partnership, or if the second parent is present at the registration (known as joint registration).
We receive birth notifications data from the NHS for linkage with birth registration records for statistical purposes. The registrar links the birth notification to the registration details at the time of registration. This linkage creates a unique sequence number which we then use to re-link the records for this birth cohort. A small number of records require us to use probabilistic linkage where this unique identifier is not available; these records are matched on a number of selected variables.
We hold the registration data on all deaths occurring in England and Wales. Routine linkage of birth records to death registration records identifies those babies who died before their first birthday.
For babies born in 2013, 698,130 live birth registration records were successfully linked to their birth notification records. This represents over 99.9% of the registration records of live births. Of these linked records, 0.07% (485) were probabilistically linked.
3,240 stillbirths were also directly linked to their birth notification using sequence number, while 6 (0.2%) records were linked probabilistically.
For infant deaths, 2,642 death registrations (99.6%) were successfully linked to their corresponding birth record.
In 2015 the NN4B series was revised from 2007 to 2012. Details of the revisions and revised tables can be found on our website.
The name of this bulletin will be changing for future releases. All future releases will be called ‘Pregnancy and ethnic factors influencing births and infant mortality’.
Back to table of contents6. Gestational age
Table 1: Births by term, England and Wales
| Births | |||
| % | |||
| Pre-Term | Term | Post-term | |
| Live (99.5% of all births) | 7 | 89 | 3 |
| Still (0.5% of all births) | 65 | 34 | 1 |
| Source: Office for National Statistics | |||
| Notes: | |||
| 1. Figures may not sum to 100 due to rounding. | |||
| 2. Known gestation only. | |||
Download this table Table 1: Births by term, England and Wales
.xls (28.2 kB)The table above shows the percentage of births in each gestational group. The pre-term gestation category can be broken down into 3 more gestation groups. Of the 7% of births that were pre-term, almost 5% were extremely pre-term (between 24 and 27 weeks), 11% were very pre-term (between 28 and 31 weeks) and 85% were moderately pre-term (between 32 and 36 weeks).
Stillbirths accounted for 0.5% of all births in 2013. Of the 3,241 stillbirths where gestational age was known, 65% were born pre-term. Of these, 39% were extremely pre-term, 25% were very pre-term and 36% were born moderately pre-term.
Figure 1 shows that the percentage of babies dying within the first year falls to below 10% in births from 28 weeks gestation onwards.
Figure 1: Percentage of infant deaths and number of live births by week gestation, 2013
England and Wales
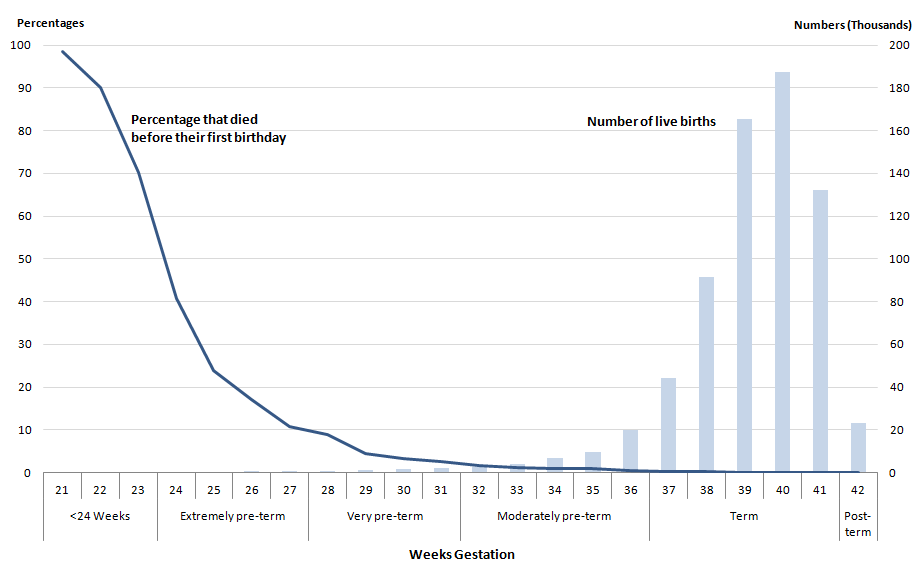
Source: Office for National Statistics
Download this image Figure 1: Percentage of infant deaths and number of live births by week gestation, 2013
.png (34.5 kB) .xls (19.5 kB)Figure 1 shows that in 2013, out of the total live births with known gestation, 1% occurred before 32 weeks gestation (earlier than moderately pre-term). Of these births 15% resulted in an infant death, which accounted for over half of all infant deaths. Almost all live births (99%) occurred at 32 weeks gestation or later, with 0.2% of these births resulting in an infant death. Infant deaths where the baby was born at 32 weeks gestation or later made up 47% of all infant deaths.
In 2013, 99% of births in the “under 22 weeks and birthweight less than 1,000g” category lead to an infant death. This decreased to 90% for births at 22 weeks gestation, and rapidly fell to less than half (41%) for 24 weeks gestation. By 27 weeks gestation (the end of the extremely pre-term category) the percentage of births that resulted in an infant death fell to 11%. The percentage of infant deaths was 1% for babies born at 34 weeks gestation. For each week from 38 weeks gestation onwards, the percentage of infant deaths fell to 0.1%. A fetus is considered viable at 24 weeks. Very few live births occur before this, and infant mortality rates for the few babies born this early are extremely high. For babies born in 2013, 0.1% of live births occurred at less than 24 weeks. The infant mortality rate for these babies was 853.5 deaths per 1,000 live births. The majority of these deaths (92%) occurred during the early neonatal period (the first week of life).
There has been little change in the distribution of birth by gestational age since 2006, when this time series was started. In the publication reporting the 2006 figures, post-term babies were reported in the same category as term babies (37 weeks and over). The report showed that 92% of babies were born after 37 weeks (term and post-term), this is the same value found in 2013.
Reference table 2 (228.5 Kb Excel sheet) shows that the infant mortality rate for babies born pre-term in 2013 was 21.1 deaths per 1,000 live pre-term births. The 2013 rate is lower, but not statistically significantly, than the rate for 2012 (23.6 deaths per 1,000 live births), the 2013 rate is significantly lower than the rate in 2006 (28.6 deaths per 1,000 live births). The rate of infant mortality of pre-term babies was significantly higher than the overall infant mortality rate (3.8 deaths per 1,000 live births). The infant mortality rate for babies born at term stayed the same as 2012 (1.4 deaths per 1,000 live births) and was significantly lower than the overall infant mortality rate. Babies born post-term (42 weeks and over) in 2013 had an infant mortality rate of 1.3 deaths per 1,000 live births, this is a non-significant rise from 2012 (0.9 deaths per 1,000 live births). The infant mortality rate for term and post-term births is significantly lower in 2013 (1.4 deaths per 1,000 live births) compared to the 2006 infant mortality rate (1.9 deaths per 1,000 live births). Recent research has indicated that babies born moderately pre-term (32 to 36 weeks) and early term (37 to 38 weeks) have an increased risk of ill health during childhood (Boyle et al., 2012).
Back to table of contents7. Ethnicity
Table 2: Births by term and ethnicity, England and Wales, 2013
| Live births | ||||||||||
| % | ||||||||||
| Bangladeshi | Indian | Pakistani | Black African | Black Caribbean | White British | White Other | All Other | Not Stated | ||
| Births | 1 | 3 | 4 | 3 | 1 | 64 | 9 | 10 | 3 | |
| Of which | ||||||||||
| Pre-term | 8 | 7 | 7 | 8 | 10 | 7 | 6 | 7 | 8 | |
| Term | 91 | 90 | 90 | 88 | 87 | 89 | 90 | 90 | 88 | |
| Post-Term | 2 | 2 | 2 | 4 | 2 | 4 | 3 | 3 | 4 | |
| Source: Office for National Statistics | ||||||||||
| Notes: | ||||||||||
| 1. Figures may not sum to 100 due to rounding. | ||||||||||
| 2. Known gestation only. | ||||||||||
Download this table Table 2: Births by term and ethnicity, England and Wales, 2013
.xls (34.3 kB)The baby’s ethnic group is taken from the birth notification and is as stated by the mother. In 2013, 73% of all live births stated their ethnicity as White British or White Other. The highest proportion of pre-term births occurred in the Black Caribbean ethnicity (10%). White British and Black African ethnicities had the highest percentage (4%) of post-term births.
There is very little research looking at birth outcomes by babies’ ethnicity, although it is likely that there is a strong relationship between the ethnicity of the baby as stated by the mother and the mother’s own ethnicity. If this is the case, the ethnicity of the mother may help to explain the differences in gestation and infant mortality between ethnic groups. Some research suggests that Black and Asian women have shorter gestation than White European women, and that this may be due to the fetus developing earlier (Patel et al., 2004). The discrepancies in gestation by ethnicity may also be explained by socio-economic, behavioural and physiological differences among the different ethnic groups (Gray et al., 2009).
Figure 2: Infant mortality rates, by ethnicity, 2013
England and Wales
Source: Office for National Statistics
Download this chart Figure 2: Infant mortality rates, by ethnicity, 2013
Image .csv .xlsWhite Other babies have the lowest infant mortality rate with 2.6 deaths per 1,000 live births. This rate was statistically significantly lower than each other ethnicity. White British babies (3.3 deaths per 1,000 live births) also had significantly lower infant mortality rates than each of the other ethnicities, except Indian (3.9 deaths per 1,000 live births). White Other and White British ethnic groups had the lowest percentage of births with low birthweight (5% and 7%, respectively); this may partially explain their lower infant mortality rates.
Pakistani, Black Caribbean and Black African babies (6.7, 6.6 and 6.3 deaths per 1,000 live births respectively) had the highest infant mortality rates. Research suggests that there is a link between lower National Statistics Socio-economic Classification (NS-SEC) group and poorer maternal health, which can have an impact on infant mortality (Oakley et. al. 2009). This may explain some of the pattern seen here as a high percentage of Pakistani births occur in the Routine and Manual NS-SEC group. Black African and Black Caribbean (who are also more likely to be pre-term) have a high percentage of births in the Other NS-SEC group. More information on NS-SEC can be found in the NS-SEC section of this bulletin and in the metadata of the reference tables (228.5 Kb Excel sheet).
Another factor affecting infant mortality rates is where the child lives. Using the index of multiple deprivation quintiles, Bangladeshi, Pakistani, Black African and Black Caribbean babies were more likely to be residents of areas of high deprivation than White British and White Other babies.
Reference table 8 (228.5 Kb Excel sheet) shows the mortality rates for different ethnicities, which are discussed with different variables throughout the bulletin.
Back to table of contents8. Birthweight
Table 3: Births by term and birthweight, England and Wales, 2013
| Live births | |||
| % | |||
| Pre-Term | Term | Post-term | |
| Low (less than 2,500g) | 62 | 37 | 0.2 |
| 2,500g and over | 3 | 93 | 4 |
| Source: Office for National Statistics | |||
| Notes: | |||
| 1. Figures may not sum to 100 due to rounding. | |||
| 2. Known gestation only. | |||
Download this table Table 3: Births by term and birthweight, England and Wales, 2013
.xls (55.3 kB)
Figure 3: Infant mortality rates for low birthweight births, by ethnicity, 2007 and 2013
England and Wales
Source: Office for National Statistics
Download this chart Figure 3: Infant mortality rates for low birthweight births, by ethnicity, 2007 and 2013
Image .csv .xlsLow birthweight, one of the known risk factors for infant deaths, can be caused by a number of factors. Babies weighing less than 2,500 grams are considered to have a low birthweight. The relationship between gestational age and birthweight is reflected in the infant mortality rates of low birthweight babies. Reference table 3 (228.5 Kb Excel sheet) of the reference tables shows that for babies born in 2013, the highest infant mortality rates occurs in the under 24 weeks and under 1,000 grams category (890.2 deaths per 1,000 births). The lowest infant mortality rate is 0.8 deaths per 1,000 births and occurs in the 4000 grams and over category for both term and post-term.
Figure 3 shows the infant mortality rate for low birthweight babies of different ethnicities in 2007 and 2013. The only ethnicity that showed a statistically significant change over the time period was White British, which has decreased from 37.0 to 29.0 deaths per 1,000 live births. Focusing on 2013 data, there are some significant differences when comparing ethnicities. Babies of Black African origin had the highest infant mortality rate at 54.1 deaths per 1,000 live births. This was significantly higher than Indian, White British, White Other and Other ethnic groups (24.2, 29.0 32.5 and 33.0 respectively). The infant mortality rate for Pakistani babies was 41.9 deaths per 1,000 live births, and this was also significantly higher than Indian and White British. Indian babies had the lowest rate of all ethnicities. Research shows that Indian babies tend to have lower birthweights (Kelly et al., 2009) and are more likely to be born earlier (Gray et al., 2009). The data in this bulletin show the same results, as the highest percentage of births for Indian babies occurs in 39 weeks compared to 40 weeks for White British and White Other.
Back to table of contents9. Age of mother at birth of baby
Table 4: Births by term and mother's age, England and Wales, 2013
| Live births | |||
| % | |||
| Pre-Term | Term | Post-term | |
| 20 and under | 8 | 89 | 3 |
| 20 to 24 | 7 | 89 | 3 |
| 25 to 29 | 7 | 90 | 3 |
| 30 to 34 | 7 | 89 | 3 |
| 35 to 39 | 8 | 88 | 3 |
| 40 and over | 11 | 87 | 2 |
| Source: Office for National Statistics | |||
| Notes: | |||
| 1. Figures may not sum to 100 due to rounding. | |||
| 2. Known gestation only. | |||
Download this table Table 4: Births by term and mother's age, England and Wales, 2013
.xls (55.8 kB)The highest percentages of term births occur in those aged 25 to 29. Those aged 40 and over have the lowest percentage of term births and the highest percentage of pre-term births. The next highest percentage of pre-term births occur in mothers aged 35 to 39 or under 20.
Infant mortality rates for term babies have fallen since 2007 for mothers of all ages, the only statistically significantly lower rates are for mothers ages 20 to 24 and 25 to 29. In 2013, the lowest infant mortality rate occurred in mothers aged 35 to 39 (1.2 deaths per 1,000 live births), while the highest rates occur in mothers aged under 20 and mothers aged over 40, 2.2 and 1.7 deaths per 1,000 births respectively. Research shows that maternal age for single births typically has a U-shaped relationship with infant mortality when plotted on a graph, with rates being highest for babies of the youngest and oldest mothers (Misra and Ananth, 2002); Pre-term and multiple births do not tend to follow the U-shaped relationship.
Mothers aged under 20 and over 35 are more likely to give birth before 37 weeks. Infant mortality rates for pre-term births have also fallen since 2007 for mothers of all ages; the decrease was significant for ages 20 to 24, 25 to 29 and 30 to 34. Mothers aged under 20 and 20 to 24 have higher pre-term infant mortality rates than older mothers for each year except 2010, where mothers aged over 40 had a higher mortality rate than those aged 20 to 24.
In 2013, the lowest infant mortality rate for pre-term births occurs in mothers aged 25 to 29 with 18.3 deaths per 1,000 live births. Mothers aged under 20 have the highest mortality rates at 32.1 deaths per 1,000 live births.
When comparing rates broken down by ethnicity, the highest rate for each ethnic group was for mothers aged under 20 or mothers aged 40 and over. Black Caribbean and White British have the highest percentage of births in under 20s, which makes up 5% of both ethnicities age breakdown.
More information can be found in reference table 4 (228.5 Kb Excel sheet).
Back to table of contents10. Multiplicity
Table 5: Births by term and multiplicity, England and Wales, 2013
| Live births | |||
| % | |||
| Pre-Term | Term | Post-term | |
| Single | 6 | 91 | 3 |
| Multiple | 57 | 43 | 0.1 |
| Source: Office for National Statistics | |||
| Notes: | |||
| 1. Figures may not sum to 100 due to rounding. | |||
| 2. Known gestation only. | |||
Download this table Table 5: Births by term and multiplicity, England and Wales, 2013
.xls (55.3 kB)
Figure 4: Infant mortality rates by multiplicity and term, 2007 and 2013
England and Wales
Source: Office for National Statistics
Notes:
- Rates for pre-term multiple births are consistently lower than singleton births. The opposite can be seen in term births.
Download this chart Figure 4: Infant mortality rates by multiplicity and term, 2007 and 2013
Image .csv .xlsAs shown in Figure 5, over the time period 2007 to 2013, for pre-term babies, infant mortality rates are consistently higher for single births compared to multiple births (18.3 and 21.9 respectively in 2013). For term babies, infant mortality rates for single births are consistently lower than multiple births (1.2 and 2.2 respectively in 2013).
A reason for this may be because single and multiple live births have very different gestational age distributions. Most women with a twin pregnancy are expected to give birth earlier (at around 36 to 37 weeks gestation) than women with a singleton pregnancy, and there may be an increased risk of stillbirth from 37 weeks for twin pregnancies (Dodd et al., 2012). Reference table 5 (228.5 Kb Excel sheet) shows 2013 neonatal and infant mortality rates for single and multiple births.
Mortality rates are higher for multiple babies born to teen mothers and lower for multiple babies born to older mothers (Misra and Ananth, 2002; Salihu et al., 2004)
Almost all ethnicities show a statistically significantly higher rate of infant death in multiple births compared to single births. Those with ethnicity of Bangladeshi and Black Caribbean show no significant difference, this may be due to these ethnicities having the lowest percentage of multiple births.
Back to table of contents11. Marital status and type of registration
Table 6: Births by term and marital status, England and Wales, 2013
| Live births | |||
| % | |||
| Pre-Term | Term | Post-term | |
| Married | 7 | 90 | 3 |
| Joint - same address | 7 | 89 | 4 |
| Joint - different address | 9 | 88 | 3 |
| Sole registration | 10 | 87 | 3 |
| Source: Office for National Statistics | |||
| Notes: | |||
| 1. Known gestation only. | |||
Download this table Table 6: Births by term and marital status, England and Wales, 2013
.xls (55.3 kB)Sole registered births and joint registration with parents living at different addresses are more likely to be pre-term than jointly registered births with parents living at the same address and at births where the parents are married.
Figure 5: Percentage of births by ethnicity and registration type, 2013
England and Wales
Source: Office for National Statistics
Download this chart Figure 5: Percentage of births by ethnicity and registration type, 2013
Image .csv .xlsNearly all ethnicities show that most registrations occur inside marriage. The exception is babies who are Black Caribbean, who are most likely to be registered jointly where the parents live at different addresses.
Maternal unmarried status is associated with an increased risk of low birthweight, pre-term birth and small for gestational age (SGA) births (Shah, Zao and Ali, 2011).
Without information about lifestyle factors, such as smoking, income and education level, it is difficult to fully explain the differences in risk of pre-term birth according to marital status. However, some of the differences in pregnancy duration may be caused by the higher prevalence of smoking among unmarried women, or greater stress during pregnancy among women in less stable relationships than married women. However, it is likely that the characteristics of the mother’s relationship to a partner are more important than the marital status itself (Luo et al., 2004).
Infant mortality rates, for babies born in 2013 with a known gestational age, were highest for babies that were sole registered (5.6 deaths per 1,000 live births), followed by babies registered by unmarried parents living at different addresses (4.7 deaths per 1,000 live births). Both of these rates were statistically significantly higher than those for babies registered by unmarried parents living at the same address and babies registered by married parents (both 3.5 deaths per 1,000 live births). The mortality rates for pre-term babies followed a slightly different pattern, with babies registered to unmarried parents living at different addresses having the highest rate (24.9 deaths per 1,000 live births), which was significantly higher than those for babies registered by married parents, with the lowest rate of 19.4 deaths per 1,000 live births.
Reference table 6 (228.5 Kb Excel sheet) shows rates for registration type by gestation.
Back to table of contents12. National Statistics socio-economic classification
Details of the second parent’s occupation are only recorded where the birth is registered inside marriage or civil partnership, or is jointly registered by both parents outside marriage. Historically, tables showing births and infant mortality by National Statistics socio-economic classification (NS-SEC) were produced using only the father’s NS-SEC. However, the most advantaged socio-economic position of the parents is likely to have a direct impact on the household, whether it derives from the mother or the second parent (ONS, 2013). Reference table 7 (228.5 Kb Excel sheet) has been produced using the more advantaged NS-SEC of either parent.
Results are presented by the 4 main groups of the NS-SEC: managerial and professional, intermediate, routine and manual, and other. Other includes students, those whose occupations were inadequately described or were not classifiable, those who have never worked and the long-term unemployed. NS-SEC is only currently calculated for 10% of births in England and Wales. Because of the small numbers in the birth categories, it was not possible to calculate reliable mortality rates.
Back to table of contents13. Cause of death groups: by gestational age and combined ethinc group
Reference table 9 (228.5 Kb Excel sheet) shows that, for babies born at term and post-term, the most common cause of infant death was congenital anomalies (41% and 55% respectively). The second most common cause group for term and post-term babies was sudden infant death as it accounted for 17% and 16% respectively of all infant deaths. We publish a separate report on unexplained deaths in infancy (sudden infant deaths). Figures for post-term babies are based on small numbers of deaths.
Reference table 10 (228.5 Kb Excel sheet) shows that for 4 of the 5 combined ethnic groups the most common cause of infant death was immaturity related conditions (Black, 53%; White, 44%; Mixed, Chinese and any other ethnic group, 42%; and those where ethnicity was not stated, 44%). For the Asian group, the most common cause was congenital anomalies (41%). A higher incidence of congenital anomalies in Asian populations is well-documented (Gray et al. 2009).
Back to table of contents14. Small for gestational age
Table 7: Births by term and SGA, England and Wales, 2013
| Live births | |||
| % | |||
| Pre-Term | Term | Post-term | |
| SGA | 9 | 8 | 7 |
| Source: Office for National Statistics | |||
| Notes: | |||
| 1. SGA is small for gestational age. | |||
| 2. Known gestation only. | |||
Download this table Table 7: Births by term and SGA, England and Wales, 2013
.xls (54.8 kB)
Figure 6: Infant mortality rates for small for gestational age babies, by ethnicity, 2011 to 2013
England and Wales
Source: Office for National Statistics
Download this chart Figure 6: Infant mortality rates for small for gestational age babies, by ethnicity, 2011 to 2013
Image .csv .xlsLow birthweight and prematurity are both measures of fetal development. Another measure is the baby’s size in relation to its gestational age. Babies whose birthweight lies below the tenth percentile for their gestational age are known as “small for gestational age” (SGA).
Not all babies who are SGA have a pathological growth restriction; they may just be physically small. This may explain why babies of Bangladeshi, Indian or Pakistani origin are more likely to be SGA than White British babies.
Indian ethnicity has the second highest percentage of SGA babies (16%), however, as shown in Figure 7, Indian babies have the lowest SGA infant mortality rate (5.9 deaths per 1,000 live births). This rate is statistically significantly lower than the rate for Black African, Pakistani and Other (15.9, 13.1 and 8.8 respectively). The highest mortality rate was for the Black African ethnicity (9% SGA births), which was significantly higher than all ethnicities except for Pakistani and Black Caribbean.
In 2013, for those born SGA, there is a significantly higher mortality rate for the early neonatal period (up to 6 days) compared to late neonatal (7 to 28 days) and post neonatal (over 28 days).The post neonatal mortality rate was also significantly higher than the rate for late neonatal deaths. The rates for early neonatal, late neonatal and post neonatal were 4.3, 1.2 and 2.9 deaths per 1,000 live births respectively.
Research shows that pre-term SGA is more closely associated with medical conditions related to pre-eclampsia, rather than with socio-demographic status, while term SGA is associated with socio-demographic status and various medical conditions (Ota et al., 2014).
A range of environmental and maternal factors also contribute to SGA. In the categories of births analysed, the following groups had the highest proportion of SGA babies: where the birth was solely registered by the mother (11%), mothers aged less than 20 years (11%), multiple births (16%) and the Bangladeshi ethnic group (17%).These are not necessarily separate (discrete) groups.
Back to table of contents
